Scanning Driven Designs

Various critical healthcare technologies and problems require the need for interfacing materials with biology. Specifically, the challenge of designing and manufacturing multi-functional form-fitting interfaces with biology is a current barrier for developing next-generation ‘smart’ biomedical devices, such as those with personalized, bio-inspired, and bionic interfaces. This challenge is rooted in the fundamental difference between the geometry of engineered and biological systems. For example, while engineered systems are typically defined by ‘geometric’ shapes (e.g., triangles or circles), biology is composed of irregular ‘organic’ shapes that are associated with the natural world. Thus, solutions to this problem requires holistic collaboration between engineers and designers. While many applications exist, we are focused on two critical areas that disproportionately affect children and the elderly – personalized prosthetics for amniotic band syndrome (ABS) and bio-inspired prosthetics for organ transplantation, respectively. The project will focus on three healthcare problems that affect both developed and underdeveloped societies worldwide as well as citizens with disabilities will significantly:
- Enhance the learning outcomes of participating students by providing expanded context
- Increase the potential to secure external funding
- Increase the national and international visibility of the project.
Birth defects associated with ABS, a common type of birth defect, typically result from the entanglement of limbs in the amniotic band in utero. The result is typically a deformed hand, arm, foot, or leg, and can result in significant loss of function and quality of life for children. The objective of this experience is to provide an interdisciplinary group of students with the opportunity to develop personalized prosthetic hands for children with ABS using a combination of light scanning and AM technology. The project will result in personalized prosthetic limbs for children in the local community with limb deformities resulting from ABS. The PI has already been approved by the VT IRB to conduct this research (#16-777).
Loss of viable organs resulting from poorly optimized transplantation conditions is a critical factor that drives the worldwide organ shortage crisis. For example, only ~20% of patients on the kidney transplantation list will receive an organ. Transplanted organs are typically transported from donor to recipient on flat rigid surfaces (typically the bottom of temperature-controlled vessels), which impedes the ability to protect, monitor, and maintain the native shape of explanted organs during the transplantation interval. As a result, transplanted organs can be rejected or even discarded altogether prior to transplantation. The objective of this experience is to provide an interdisciplinary group of students with the opportunity to develop form-fitting prosthetics for kidney transplantation, also referred to as ‘organ sleeves.’ The project will result in bio-inspired organ prosthetics to increase the number of quality kidneys available for organ transplantation. The PI has already been approved by the VT IBC to conduct this research (#16-039).
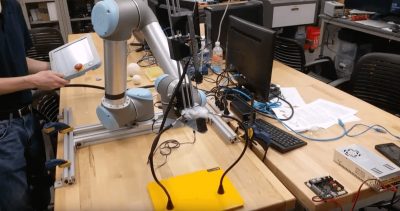
Both experiences involve collaboration between students from engineering and industrial design backgrounds. Students will: 1) image deformed limbs and whole organs using light scanning systems; 2) design prosthetic interfaces in computer-aided design environments; 3) fabricate prosthetic devices using AM processes; and 4) assess prosthetic performance using light scanning techniques. Importantly, given that these experiences contain an assessment phase that involves participants (children ranging ~5-17 years of age) and animal tissues (adult porcine kidneys), the research involves a valuable feedback loop that enhances the student learning outcomes and provides technology optimization (further details provide under research strategy).
This will be the first research to our knowledge that unites 3D structured-light scanning design techniques with multi-material AM processes toward the development of personalized, bio-inspired ‘smart’ interfaces for internal and external tissues.
Experience 1: Scanning-driven Design, AM, and Assessment of Personalized Prosthetics for Children with ABS:
This experience will begin with design and end with delivery, usage, and assessment. Participants have already been identified for the project consisting of children from the New River Valley area. Ongoing collaboration with the world’s largest organization for disabled persons (www.Jaiperfoot.org) will also be leveraged to identify additional international participants (maximum of three) in underdeveloped societies that require load-bearing prosthetics. The potential impact of this project on children in emerging economies can be significant. As digital scanning tools become more common, we can potentially help Jaiperfoot create a much more efficient method for creating custom prosthetics where 3D scanning can eliminate the need to create plaster molds of the child’s stump, thereby reducing cost. Importantly, the 3D printed prosthetics have a total cost of ~$20 USD, which compares reasonably with those utilized in underdeveloped regions that typically cost ~$25,000 Indian rupees (~$40 USD). In fact, a saving of ~ $20 per prosthetic can allow hundreds to thousands of children to receive prosthetics that otherwise might not.
We will begin the experience by conducting an initial interview of the participant (and the participant’s parents or guardians) in the office of the PI. The time commitment is ~ 1 hour. This interview will determine what baseline prosthetic design to use from an online database for ABS prosthetics established by the non-profit global network organization e-NABLE (www.enablingthefuture.org). Following the initial interview, the digital model for the baseline prosthetic will be downloaded and fabricated using commercially available plastic 3D printers (e.g., Makerbot). The prosthetic will then be assembled using a commercially available assembly kit (also available from e-NABLE). Subsequently, the non-personalized prosthetic will be delivered to the participant. We will then ask the participant to test the prosthetic for a period of two weeks to assess comfort, design and functionality.
Following the initial testing period, a second interview will be conducted. This will allow the participant to provide feedback on the baseline prosthetic. This data serves as a control for the study, as the baseline prosthetic lacks personalization. During the second interview (Location: Laboratory of the PI in the Corporate Research Center 2270 Kraft Dr. Room # 1307; Time Commitment: ~ 1 hour), the participant’s limb will be scanned via a commercially available non-contact structured-light scanning systems (SLS-2 by David Vision and ExaScan by Creaform). This will generate a digital model that captures the geometric shape of the ABS defect. This data will then be utilized to design and introduce a personalized interface into the baseline prosthetic using computer-aided design software (Solidworks). In other words, it will achieve an optimal match between the prosthetic’s interior surface and the participant’s limb. The personalized prosthetic will then fabricated and assembled. We will then ask the participant to test the prosthetic for a period of two weeks to assess comfort, design and functionality.
A third interview will then be conducted to assess the performance of both prosthetics (the personalized prosthetic and the baseline model, which serves as a control). During the third interview, the participant will be asked to perform common tasks (e.g., grasping), and the functional performance will be qualitatively assessed through photography, videography, and survey questions. Subsequently, we will conduct light scanning-based measurements of the dynamic range of prosthetic motion to quantitatively assess the range of motion that the child is capable of generating. The total duration of this experience will be ~ 3 months per participant.
Upon completion of the experience, the participant may continue to use the prototypes under parental and physician supervision. Continued support and maintenance of the prosthetics beyond this experience will not be provided at this time. The participants are allowed to keep the prosthetics upon completion of the project. Continued use will be governed by the participant's physician. Importantly, we have already run a pilot study led by a team of four undergraduate students that delivered a prosthetic hand to a child in our local community (see Figure 1). The pilot study received coverage from local media outlets, including FOX and NBC.
Experience 2: Scanning-driven Design, AM, and Assessment of Bio-inspired Prosthetics for Organ Transplantation:
This experience will begin with design and end with testing on whole organs explanted from adult porcine kidney models (i.e., pig kidneys). The geometric design of the organ prosthetics will be accomplished by generating digital models of native organ geometry using 3D structured light scanning techniques. Dimensional accuracy of digital models will be validated against physical model controls. The digital models serve to provide: 1) a digital template for AM of the organ prosthetic; and 2) a computational domain for understanding the influence of the prosthetic on the organ deformation under body forces.
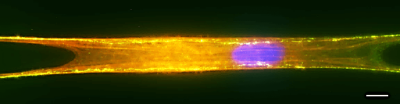
Modeling of prosthetic-organ adhesion phenomena and component flexibility will be leveraged to understand the mechanical compatibility and bonding between potentially integrated sensor materials under dynamic strains that occurs during perfusion of solid organs. Finite element analysis will be used to: 1) understand the mechanical stabilization provided by the organ prosthetic; 2) apply the concepts of kirigami art-forms to design configurations and features required to maintain mechanical integrity between the prosthetic and organ; and 3) inform the position of integrated sensors for mechanical strain and pressure measurement. Once the prosthetic has been manufactured, the stability under dynamic loading will be assessed under gravity perfusion via light scanning. Importantly, we have already run a pilot study involving one undergraduate student that delivered a prosthetic patch for organ monitoring (see Figure 1). The pilot study was highlighted as the cover of the journal Lab on a Chip (Impact factor ~ 7).
The ability to customize the interface between prosthetics and arbitrary internal and external tissues will advance the field of biomedical device design and manufacturing. For example, the ability to personalize prosthetics for ABS defect could have a significant impact on improving the aesthetics, function, and comfort of prosthetic devices, thereby improving the experience of the participant through cultivating a positive attitude towards use in social environments. Similarly, the ability to match prosthetic design to native organ geometry will provide novel opportunities for organ transplantation, such as the monitoring and quality control of organs during transplantation. Overall, this work will unify students in the design arts, life sciences, and engineering toward the development of next-generation solutions for interfacing engineered systems with biology.